Suicide Prevention Among Special Populations
Suicide affects all populations, including individuals of different races, ethnicities, sexual orientations, occupations, or ages, and there may be differences in the thoughts, behaviors, risk, and protective factors associated with suicide risk among these different groups. Additionally, various populations differ in their access to culturally appropriate behavioral health treatment, experiences of discrimination and historical trauma, and other factors that may be related to suicide risk.1 Understanding these differences is essential for more effectively directing suicide prevention and treatment efforts. Montana is a very diverse state that is made up many different populations of people. In Montana, the 5 largest ethnic groups are White (Non-Hispanic), American Indian & Alaska Native (Non-Hispanic), White (Hispanic), Two or More Races (Non-Hispanic), and Asian (Non-Hispanic).
American Indian and Alaska Natives
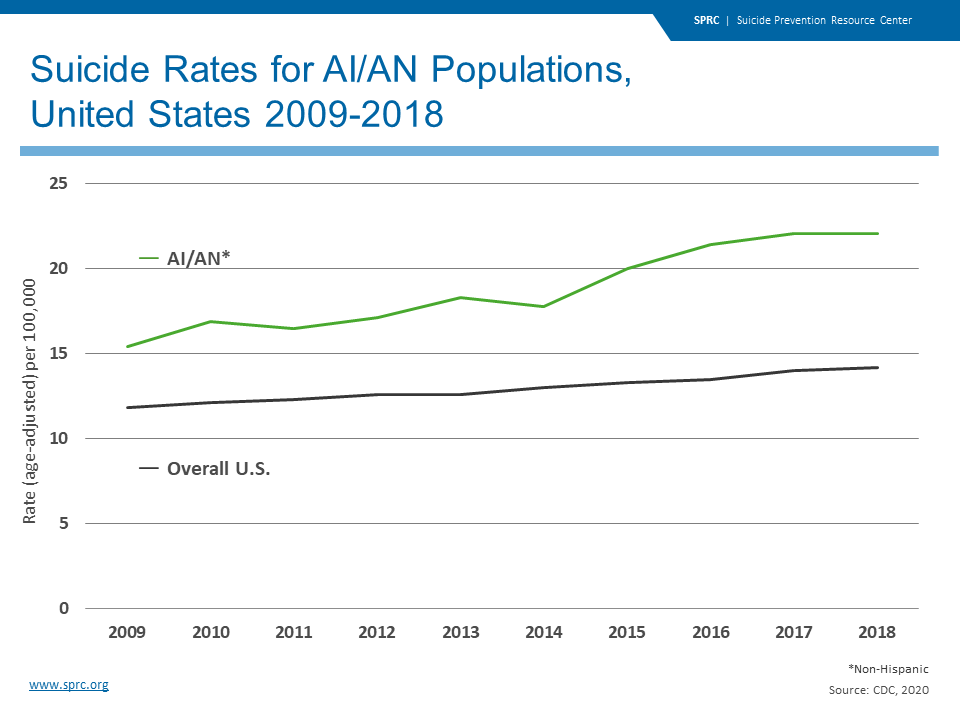
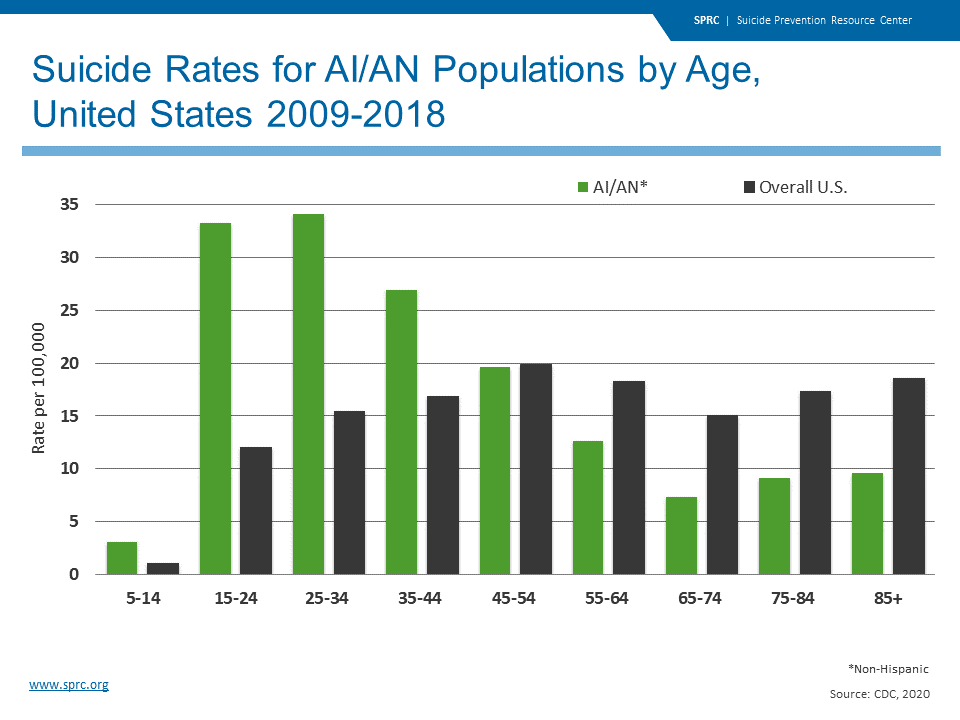
American Indians and Alaska Natives make up less than 2% of the United Stated population, yet in Montana, they are approximately 6.7 % of the state’s population. Montana is among the top 5 states with the highest proportion of American Indians and Alaska Natives. The suicide rate among American Indians and Alaskan Natives is 22.1 per 100,000, which is higher than the national rate of 14.2 per 100,000 and higher than any other racial of ethnic group in the United States.2
American Indians and Alaskan Natives encompass many ethnic and cultural groups, tribes, and traditions. This results in a number of challenges to consider to understand suicide rates in American Indian and Alaska Native populations, including:
- State mortality data often do not capture tribal affiliation.
- Tribes may have their own surveillance systems and/or their own definition of suicide.
- The concept of “suicide” may not be part of the cultural vocabulary of some tribes, making it difficult, if not impossible, to obtain rates.
- Tribes may be reluctant to share data because they fear it will be misused.2
There are a variety of risk and protective factors that should be considered when addressing suicide prevention among American Indian and Alaskan Native populations.
Risk Factors:
- Prior suicide attempt
- Mood or anxiety disorders
- Alcohol and drug use
- Historical trauma (forced relocation, removal of children, outlawing of traditional religious practices, prohibiting native language and cultural traditions)
- Access to lethal means
- Triggering events (breakup, work problems, financial struggles, worsening health, etc.)
Alcohol and drug use is common among the American Indian and Alaska Native populations. According to the National Violent Death Reporting System 2003–2009, of AI/AN suicide decedents tested for alcohol, 36% were legally intoxicated at the time of death.3 In 2011, AI/AN populations had the highest rate of current illicit drug use (13.4%) among those ages 12 or older compared to any other single racial/ethnic group.3
Protective Factors:
- Effective mental health care
- Connectedness to individuals, family, communities, and social institutions
- Cultural continuity (presence of cultural facilities, self-government, having title to their traditional lands, the provision of services within the community, education, police, and fire, health care delivery, and child and family services)
- Spirituality
- Cultural identification
Approach to Suicide Prevention Among American Indian and Alaska Native Populations
Communities, local governments, organizations, etc., should draw on the strengths within Native traditions, ensuring the model for suicide prevention meets this population’s unique cultural needs. This includes promoting culturally competent practices that increase protective factors and reduce risk factors. The Suicide Prevention Resource Center created a guide for culturally competent approaches here: https://www.sprc.org/keys-success/culturally-competent. Working with the Elders and community members can be a great way to gain knowledge and understand the issues of suicide in the specific community you are working.4
Resources
- Zero Suicide in Indian Country:https://zerosuicide.edc.org/toolkit/toolkit-adaptations/indian-country
- Suicide Prevention Resource Center https://www.sprc.org/scope/racial-ethnic-disparities/american-indian-alaska-native-populations
- www.samhsa.gov/sites/default/files/topics/tribal_affairs/ai-an-data-handout.pdf
- https://www.sprc.org/keys-success/culturally-competent
Veterans
Suicide is a very important issue affecting military service members and veterans. Research suggests that up to 22 veterans die from suicide each day.1 In order to address suicide among veterans and military personnel, we must help reduce their risk for suicide before it reaches the point of crisis and support those who are in crisis.
- In 2016, the suicide rate was 1.5 times greater for veterans than for non-veteran adults, after adjusting for age and gender.2
- In 2016, 69.4% of Veteran suicides resulted from a firearm injury. In comparison, among U.S. non-Veteran adults, 48.4% of suicides resulted from a firearm injury in 2016. (Page 6)
- In Montana, the Veteran suicide rate is significantly higher than the national veteran suicide rate and the national suicide rate.
Risk Factors:
- mood and anxiety disorders
- alcohol and drug abuse
- prior suicide attempt
- physical health problems
- post-traumatic stress disorder
- stressful situations (childhood trauma, relationship problems, legal issues, financial troubles)
Protective Factors:
- social connectedness
- life skills training (financial management, communication, marriage and family relationships, conflict resolution)
- effective care for mental and physical health problems
Resources
- Army Suicide Prevention Program:https://www.armyresilience.army.mil/suicide-prevention/
- Veterans Crisis Line: Provides information to call, text, or chat online with a trained responder. https://www.veteranscrisisline.net/
- Military Crisis Line: Provides a hotline, text service, and online chat with a trained responder for those in the military, including veterans. https://www.veteranscrisisline.net/get-help/military-crisis-line
References:
- Kemp J., Bossarte, R. (2012). Suicide data report, 2012: Department of Veterans Affairs Mental Health Services Suicide Prevention Program. Retrieved from http://www.va.gov/opa/docs/suicide-data-report-2012-final.pdf.
- https://www.mentalhealth.va.gov/docs/data-sheets/OMHSP_National_Suicide_Data_Report_2005-2016_508.pdf
LGBTQIA+
It is evident in many ways that the LGBTQIA+ population experiences many prejudices and discriminations. This can lead to a high prevalence of social isolation, depression, anxiety, family rejection, bullying, harassment, and mistreatment. Research also shows that alcohol misuse and abuse, mental health problems, drug use, and suicidal thoughts and behaviors are more among the LGBTQIA+ populations compared to the general population.1
Risk Factors:
- Depression or other mental health conditions
- Alcohol and drug use
- Stress from prejudice and discrimination (family rejection, harassment, bullying, violence)
- Feelings of social isolation
Protective Factors:
- Family acceptance
- Sense of safety
- Connections to friends and others who care about them
Resources
Mental Health providers can learn how to better understand the LGBTQIA+ population in order to provide more appropriate care to them.
- Video on how to provide more culturally competent care to LGBT youth
- Workshop that trains professionals who serve youth on how to prevent suicide among LGBT youth. This training is beneficial for teachers, social welfare staff, clergy, group home staff, juvenile justice staff, foster parents, therapists, school administrators, recreation workers, etc.
- Talking About Suicide and LGBT Populations is an important resource for that provides facts and misconceptions about suicide among the LGBT population, including guidelines for talking about suicide in safe and accurate ways.
- Family Acceptance Project: works to prevent health and mental health risks among LGBT children and youth in the context of their families and communities.
- FAP's research shows that families, parents, foster parents, caregivers, and guardians can have a very dramatic impact on their LGBT children. It found that family acceptance promotes well-being and helps protect LGBT young people against risk and that family rejection has a serious impact on a gay or transgender young person's risk for health and mental health problems, such as depression, suicide, substance abuse and HIV.
- Trans Lifeline is a free crisis hotline staffed by transgender people for transgender people: (877) 565-8860.
- The Trevor Project is a national organization focused on crisis and suicide prevention efforts among lesbian, gay, bisexual, transgender and questioning (LGBTQ) youth. The Trevor Project operates the only accredited, nationwide, around-the-clock crisis and suicide prevention helpline for LGBTQ youth.
References
- Haas, A. P., Eliason, M., Mays, V. M., Mathy, R. M., Cochran, S. D., D’Augelli, A. R. . . . Clayton, P. J. (2011). Suicide and suicide risk in lesbian, gay, bisexual, and transgender populations: Review and recommendations. Journal of Homosexuality, 58(1), 10–51.
Farming and Agriculture
Suicides among farmers has become a major public health concern in recent years. The U.S. Centers for Disease Control and Prevention figures have shown that American workers in the farming, fishing, and forestry industries have some of the highest suicide rates of any professional group.1 Suicides among farmers are 1.5 times higher than the national average.1 There are a variety of reasons suicide rates are higher in rural areas and among farmers, including sporadic access to mental health services, less overall earnings, and lower overall health factors.2 Another major factor is gun ownership. More people own and use guns per capita in rural or farming areas than the general public. Stress is often higher among farmers due to factors out of their control, such as fluctuating crop prices, weather, interest rates on land and loans, and difficulty finding good laborers.2
Resources
Farm Stress Training – Rural Resilience: This training teaches participants to recognize the signs and symptoms of stress and suicide, ways to effectively communicate with people under stress, and how to reduce stigma related to mental health concerns.
Mental Health First Aid: Mental Health First Aid offers training to teach people how to notice and respond to signs of mental health and addiction challenges with a specific focus on the cultural and environmental factors related to life in rural areas.
Farm Aid Farmer Hotline: 1-800-FARM-AID (1-800-327-6243)
References
- https://www.cdc.gov/media/releases/2018/p1115-Suicide-american-workers.html
- https://talkbusiness.net/2019/05/cdc-farm-stress-suicides-a-rising-rural-health-concern/
Additional Resources
Creating Linguistically and Culturally Competent Suicide Prevention Materials: The California Mental Health Services Authority created this guide on how to develop culturally and linguistically competent suicide prevention materials if you are an organization working with diverse communities and populations.

